The Ebola crisis of 2014 was one of the worst infectious disease outbreaks in recent history. It also occurred in a region with endemic medical risks and poor medical infrastructure. These two factors make it an important learning exercise for the global petroleum community. This paper reviews the Ebola outbreak from the viewpoint of an onshore and offshore petroleum operator, providing insight into the real threats the outbreak presented by looking past the media hype and diving into the real organizational effects of the outbreak.
Introduction
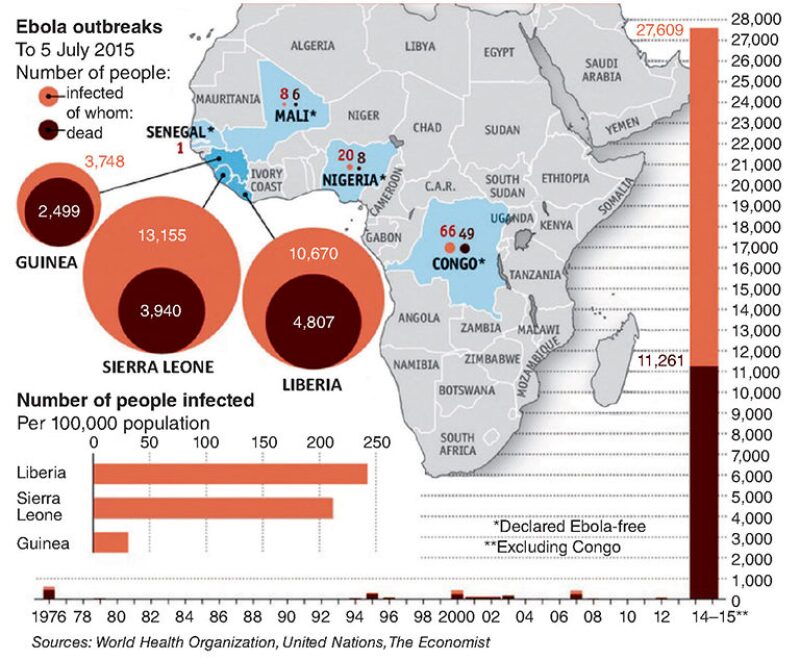
West Africa experienced the most severe Ebola virus disease (EVD) outbreak ever recorded.
×


Continue Reading with SPE Membership
SPE Members: Please sign in at the top of the page for access to this member-exclusive content. If you are not a member and you find JPT content valuable, we encourage you to become a part of the SPE member community to gain full access.